2025-12-28
2025-12-28 Share
Share
With significant steps in ASEAN countries’ collaborative efforts to advance healthcare and address the challenges of cancer, the 6th ASEAN International Forum on Integrative Oncology has successfully concluded. This grand event, bringing together numerous experts and scholars in the field of oncology from the ASEAN region and globally, like a bridge connecting cutting-edge concepts with clinical practice, injecting continuous new momentum into the development of cancer treatment. Dr. Vijaendreh Subramaniam, President of the Integrated Cancer Care Centre (ICCM) of Malaysia, delivered a highly anticipated content entitled “The Transformation of Integrative Oncology: A Malaysian Perspective,” offering a new framework for understanding the future of cancer treatment. With his years of deep expertise and rich experience in integrative oncology, his insightful and inspiring remarks at the forum are worthy of our further review and reflection.
I. Achievements and Limitations of Classic Oncology
Professor Vijaendreh Subramaniam pointed out that oncology in Malaysia and gobally followed the “classic triad ”: surgery, chemotherapy, radiotherapy—protocol-driven, standardized, universal. This model is process-oriented and characterized by highly standard, which shows four typical characteristics:
● Cancer viewed mainly as a local disease to be “cut, burned, or poisoned”—focus on tumor eradication, not on patient individuality.
● Protocols from Western centers shaped Malaysian practice; supportive or holistic care was rarely considered.
● Success meant tumor shrinkage or remission—little discussion on quality of life or personal context.
● Early training: Master the protocols, trust the algorithm, treat the tumor.

(Dr Vijaendreh Subramaniam delivering his speech )
Although some patients experience true long-term cure with classic approaches—especially with early-stage disease, its limitations are becoming increasingly apparent in clinical practice in Asian countries such as Malaysia. Dr. Vijaendreh Subramaniam stated that over 60% of cancer patients in Malaysia are are detected at Stage III or IV, and classic protocols offer little hope of cure or long-term control.
The limitations of this diagnostic and treatment system are mainly reflected in two aspects: on the one hand, management rarely (if ever) include deep molecular or immune profiling; on the other hand, Most protocols mandate fixed cycles (e.g., “6 for all”), regardless of response or toxicity.
The severity of the clinical outcomes is alarming: treatment toxicity can even become a significant factor affecting quality of life and survival time: the five-year survival rate for lung cancer in Malaysia is less than 15%, for colorectal cancer it is about 18%, and for breast cancer it is less than 50% (GLOBOCAN 2023). Even more alarming is that up to 27% of advanced cancer patients die within 30 days of palliative chemo—often from treatment, not the cancer itself.
The difficulties of treatment are becoming increasingly prominent: chemotherapy/radiotherapy contributes only 2-20% to long-term survival in adults; patients' quality of life is significantly reduced due to frequent hospitalizations, severe side effects, and emotional and economic stress; doctors and families often face the dilemma of whether continuing treatment may bring toxic risks or stopping treatment may lead to self-blame.
These data clearly show that this “one-size-fits-all” standardized treatment plan rarely takes into account factors such as tumor genetics, biological characteristics, and individual patient risks. Although it may be effective for some patients, it leaves many patients with a heavy burden of limited efficacy, significant harm, and unmet needs.
II. The Rise, Practice, and Evidence of Integrative Oncology
The challenges of clinical reality have spurred the exploration of new paradigms. Dr. Vijaendreh Subramaniamh shared a key turning point: In the early 2010s, a patient with advanced breast cancer declined further chemotherapy and instead pursued high-dose intravenous vitamin C and bio-oxidative therapies; against prevailing medical advice. Unexpectedly, the patient not only survived but also lived with quality and stability for over a decade—defying expectations.
This case has fostered an integrative medicine philosophy centered on treating the “whole patient,” emphasizing that while focusing on the tumor itself, it is even more important to consider the patient's biological characteristics, bodily defense mechanisms, and environmental factors. This integrative model organically combines traditional treatments (surgery, chemotherapy, radiotherapy, etc.) with rehabilitation support (nutritional therapy, metabolic regulation, psychological counseling, etc.) to achieve synergistic effects.
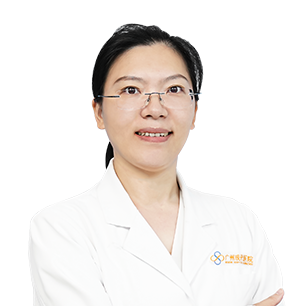
The effectiveness of this approach is supported by clinical data. Dr. Vijaendreh Subramaniamh presented results from a prospective study conducted in 2023, which included 40 patients with advanced or recurrent ovarian cancer. The data showed that the five-year survival rate was 75% in the group receiving only complementary and alternative medicine (CAM), 55% in the CAM combined with limited chemotherapy group, and 0% in the chemotherapy-only group. This demonstrates that structured, integrated approaches can provide better survival benefits and quality of life for patients with poor prognoses.
III. Synergy between Precision Medicine and Integrative Medicine
Despite the improved outcomes with integrative care, Dr. Vijaendreh Subramaniam observed a significant increase in patients with more aggressive “turbo-type cancers” in Southeast Asia post-pandemic, with some patients experiencing rapid disease progression even under integrative approaches. In response, Dr. Vijaendreh proposed a “fusion pathway of precision medicine and integrative therapy.”
Precision medicine transcends the limitations of traditional “one-size-fits-all” treatment models by analyzing the unique molecular and biological functional profiles of each patient's cancer. Utilizing oncogene and biological function analysis, it enables the matching of precise targeted therapies or biotherapies to patients at the appropriate time. This innovative approach achieves a shift from "process-oriented" to "data-driven" precision personalized treatment.
Dr. Vijaendreh illustrates the synergistic effect of precision and integration through two case studies from 2024:
Case 1: HER2-positive breast cancer patient
Precise analysis revealed that the patient was HER2-positive, PD-L1-positive, and had a functional disorder. This patient, who had previously undergone a total mastectomy and delayed chemotherapy, developed multiple metastases to the spine, liver, and lungs in 2024. Based on this, a personalized treatment plan skillfully combined targeted therapy and biological therapy, supplemented by continuous metabolic and physiological support. Ultimately, the patient successfully achieved complete metabolic remission (CR) and regained a good quality of life.
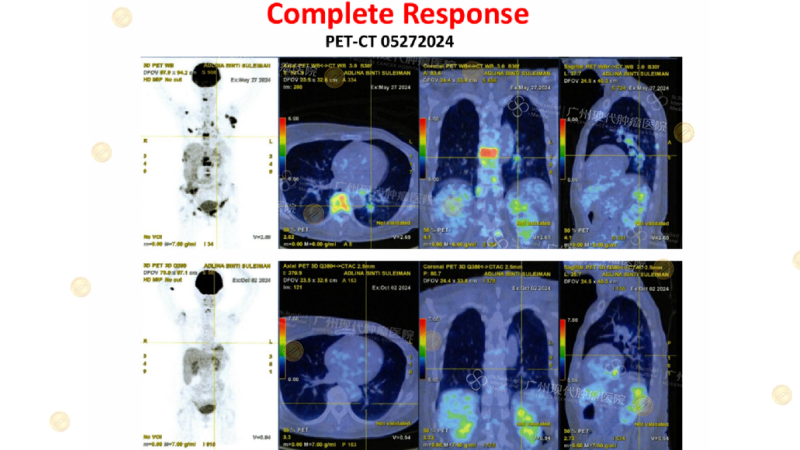
(CT shows complete disappearance of the tumor lesion)
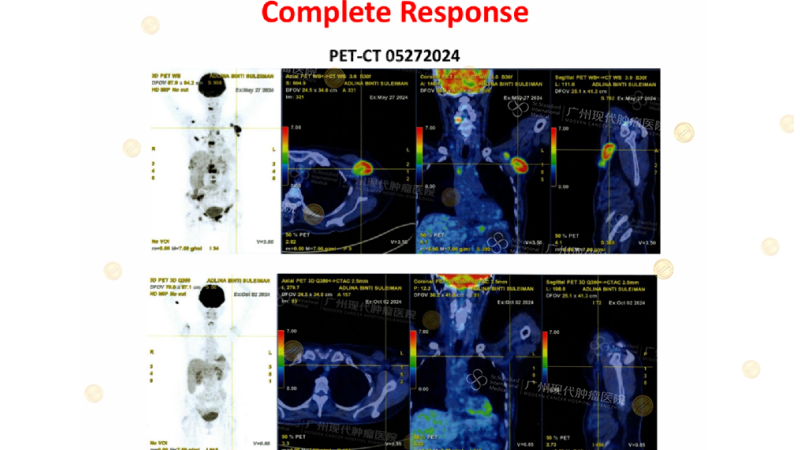
Case 2: A Patient with Refractory Ovarian Stromal Sarcoma
This 48-year-old patient with ovarian stromal sarcoma had metastasized to most of her liver and both lungs after failing multiple lines of chemotherapy. Precision diagnosis showed high expression of VEGFR2, FGFR3, and c-MET in her tumors, accompanied by significant biological dysfunction. Following a combination of biotherapy, targeted drugs, and supportive care, the patient's tumor rapidly shrank and she entered remission.
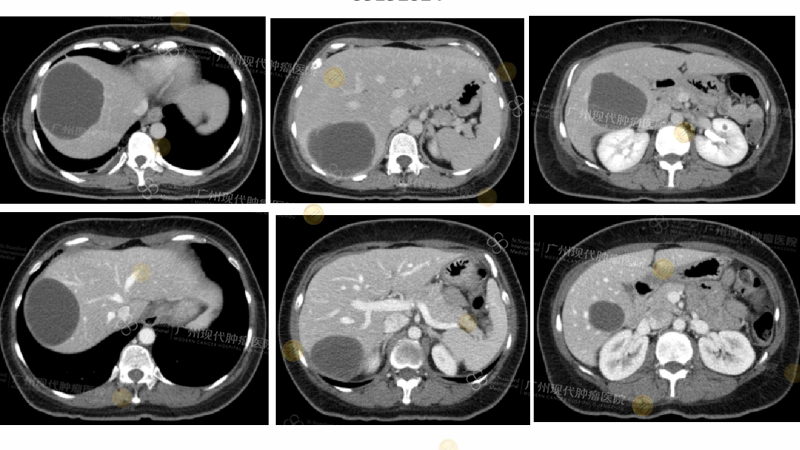
(CT shows complete disappearance of the tumor lesion)
Dr. Vijaendreh Subramaniam emphasizes that “integration is not a replacement, but an enhancement.” Integrative therapy optimizes the efficacy and tolerability of precision medicine through nutritional, metabolic, and physiological support. International consensus guidelines, such as the ASCO/SIO 2023 guidelines, have explicitly recommended integrative oncology as an important component of best practices for all cancer patients, including those receiving precision medicine.
IV. Conclusion: Towards the Future of Integration and Innovation
In his concluding remarks, Dr. Vijaendreh Subramaniam emphasized that in the face of increasingly complex cancer types and the trend of younger patients, oncology practice must evolve with the times. He pointed out the urgent need to systematically integrate traditional treatments, integrative medicine, and precision medicine. We deeply agree with Dr. Vijaendreh Subramaniam’s concept of integrative medicine, which aligns perfectly with our hospital’s long-standing practice of a “multidimensional integration, precise individualization” treatment model. We firmly believe that the future of oncology lies not in seeking a single breakthrough, but in the intelligent integration of the diverse advantages of traditional treatments, precision medicine, and integrative medicine.

In practice, Guangzhou Modern Cancer Hospital is committed to building an integrated medical system encompassing precision targeting, biological function regulation, and metabolic support, promoting the transformation of cancer treatment from “treating the tumor” to “treating the person.” We deeply understand that true treatment success lies not only in eliminating lesions, but also in helping patients regain dignity and quality of life.
The consensus reached at this conference reinforces our belief that the future of oncology will inevitably move towards a diversified and integrated development path. Guangzhou Modern Cancer Hospital is willing to join hands with global medical colleagues, using “integrative medicine” as our vessel and “innovation” as our sail, to jointly promote a profound transformation in cancer treatment from a single biomedical model to a comprehensive “bio-psycho-social” model. We look forward to gathering global wisdom through continuous international exchange and cooperation, exploring new paradigms for cancer diagnosis and treatment that are more humane and therapeutically effective, and contributing Chinese strength to the global fight against cancer.