Nasopharyngeal carcinoma
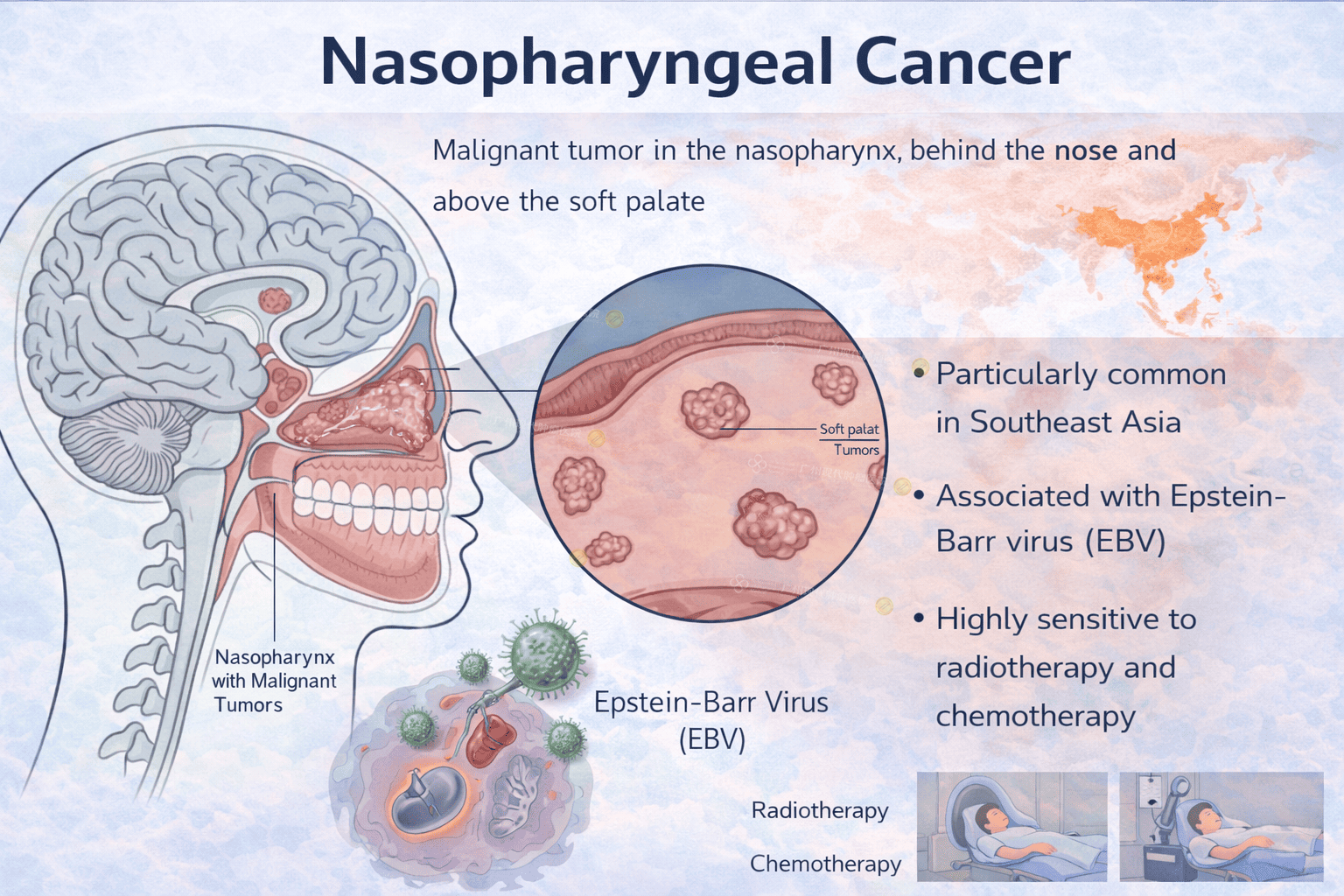
Nasopharyngeal cancer is a malignant tumor that arises from the nasopharynx, the upper part of the throat located behind the nose and above the soft palate. It behaves very differently from other head and neck cancers and has a unique epidemiology, risk profile, and treatment approach.
NPC is particularly common in Southeast Asia, including Malaysia, Southern China, Hong Kong, and parts of North Africa. Because early symptoms are subtle and non-specific, many patients are diagnosed at a locally advanced stage, but the good news is that NPC is highly sensitive to radiotherapy and chemotherapy.
Nasopharyngeal cancer originates from the epithelial lining of the nasopharynx. Unlike oral or laryngeal cancers, NPC is strongly associated with Epstein–Barr virus (EBV) infection and has a marked genetic and environmental component.
The nasopharynx is a hidden anatomical area, which explains why early tumors may grow silently without obvious symptoms.
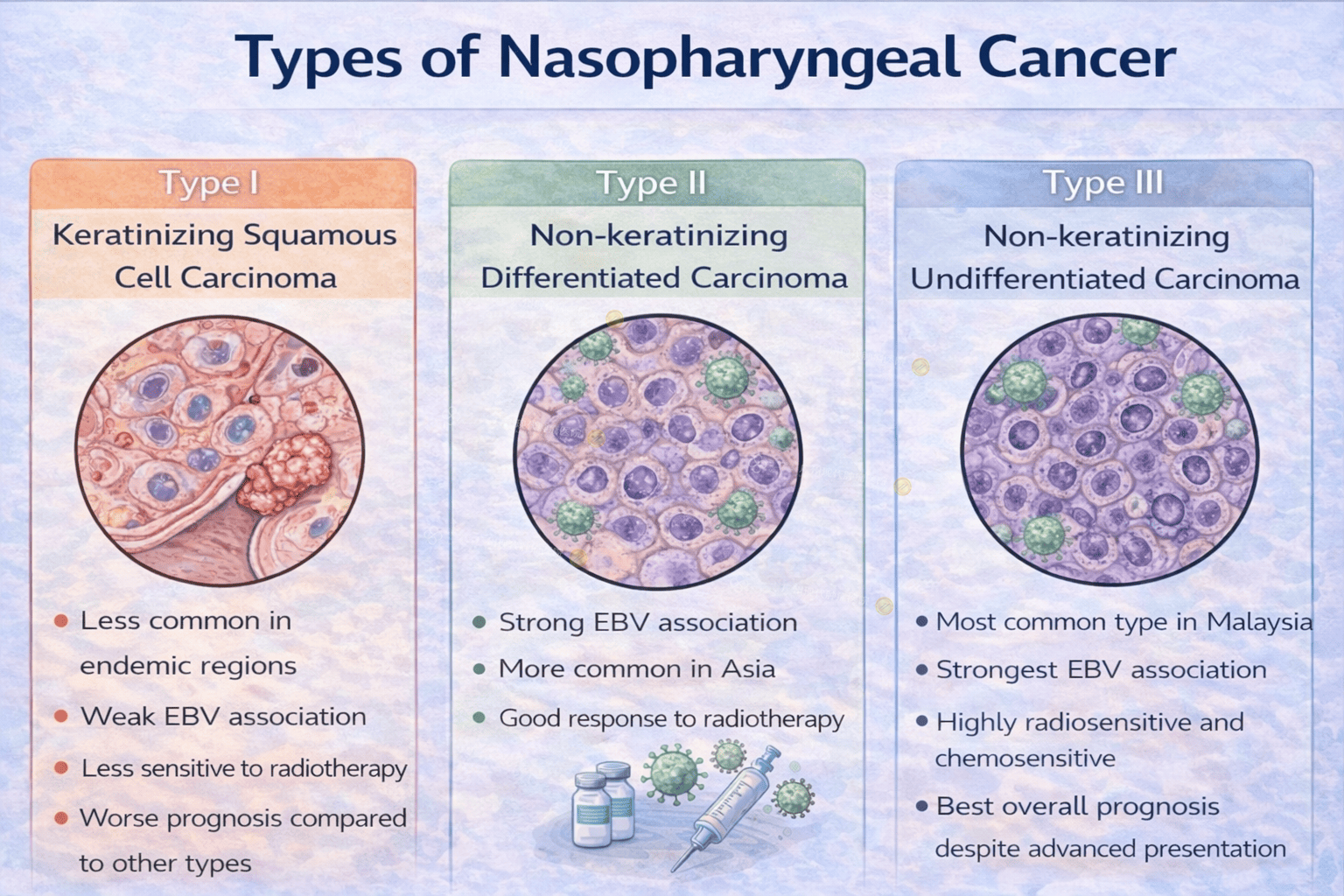
Types
Type I – Keratinizing Squamous Cell Carcinoma
Less common in endemic regions
Weak EBV association
Less sensitive to radiotherapy
Worse prognosis compared to other types
Type II – Non-keratinizing Differentiated Carcinoma
Strong EBV association
More common in Asia
Good response to radiotherapy
Type III – Non-keratinizing Undifferentiated Carcinoma
Most common type in Malaysia
Strongest EBV association
Highly radiosensitive and chemosensitive
Best overall prognosis despite advanced presentation
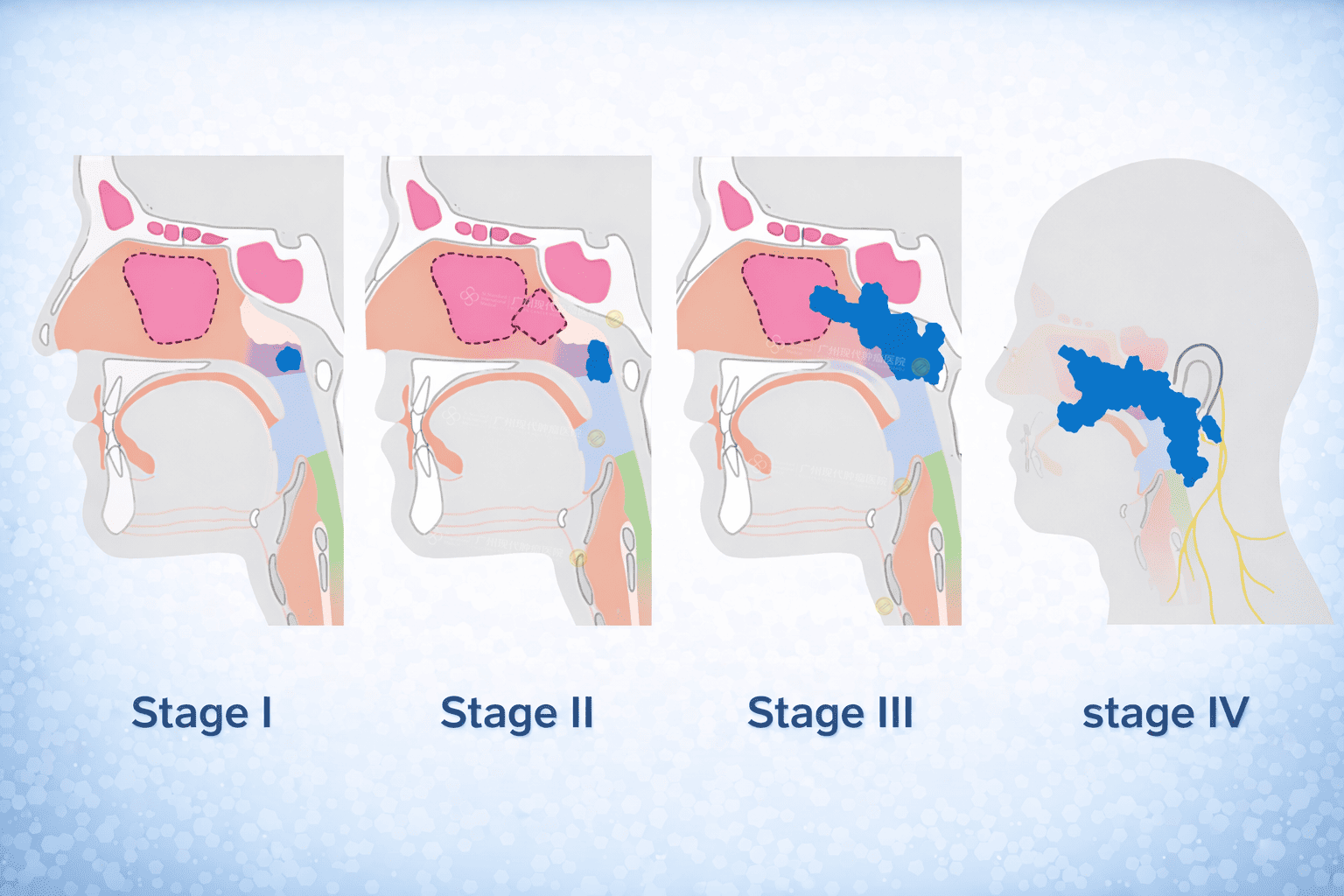
Stages
NPC is staged based on:
T (Tumor size and local invasion)
N (Regional lymph node involvement)
M (Distant metastasis)
Stage I
Tumor confined to nasopharynx
No lymph node involvement
Stage II
Extension to nearby soft tissues
Unilateral cervical lymph nodes
Stage III
Larger tumor or bilateral lymph node involvement
Stage IV
Skull base, cranial nerve invasion
Distant metastasis (bone, lung, liver)
Many NPC patients are diagnosed at Stage III or IV, yet still have good long-term survival with proper treatment.
Risk Factors
Major Risk Factors
Epstein–Barr virus (EBV) infection
Genetic susceptibility (family history)
Southern Chinese / Southeast Asian ethnicity
Environmental & Lifestyle Factors
Salted fish and preserved foods (nitrosamines)
Smoking
Alcohol (less significant than in other head & neck cancers)
Occupational exposure (wood dust, formaldehyde)
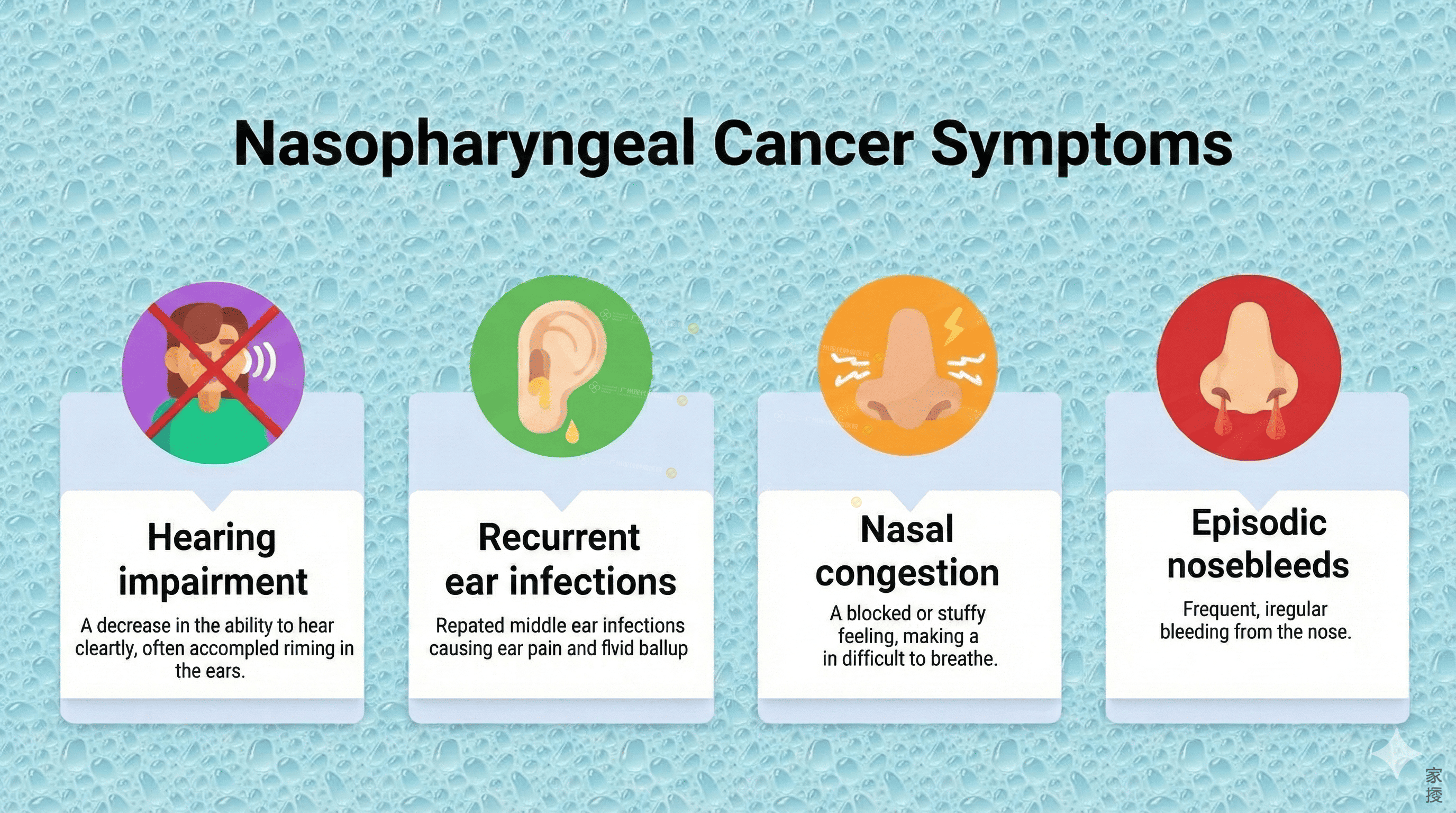
Symptoms
Early Symptoms (Often Ignored)
Persistent nasal blockage
Blood-stained nasal discharge
Ear fullness or unilateral hearing loss
Recurrent middle ear effusion (especially in adults)
Advanced Symptoms
Painless neck lump (cervical lymph nodes)
Headache
Facial numbness
Diplopia or cranial nerve palsy
Difficulty swallowing
Weight loss
A painless neck mass is one of the most common first presentations.
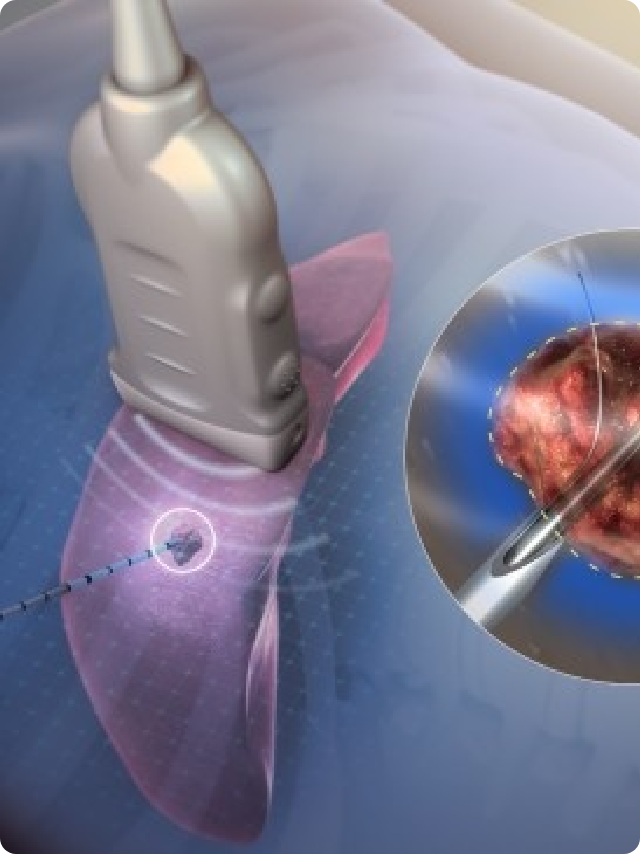
 https://img.asiancancer.com/uploads/allimg/2026/01/17/1-162948259.png
https://img.asiancancer.com/uploads/allimg/2026/01/17/1-162948259.png
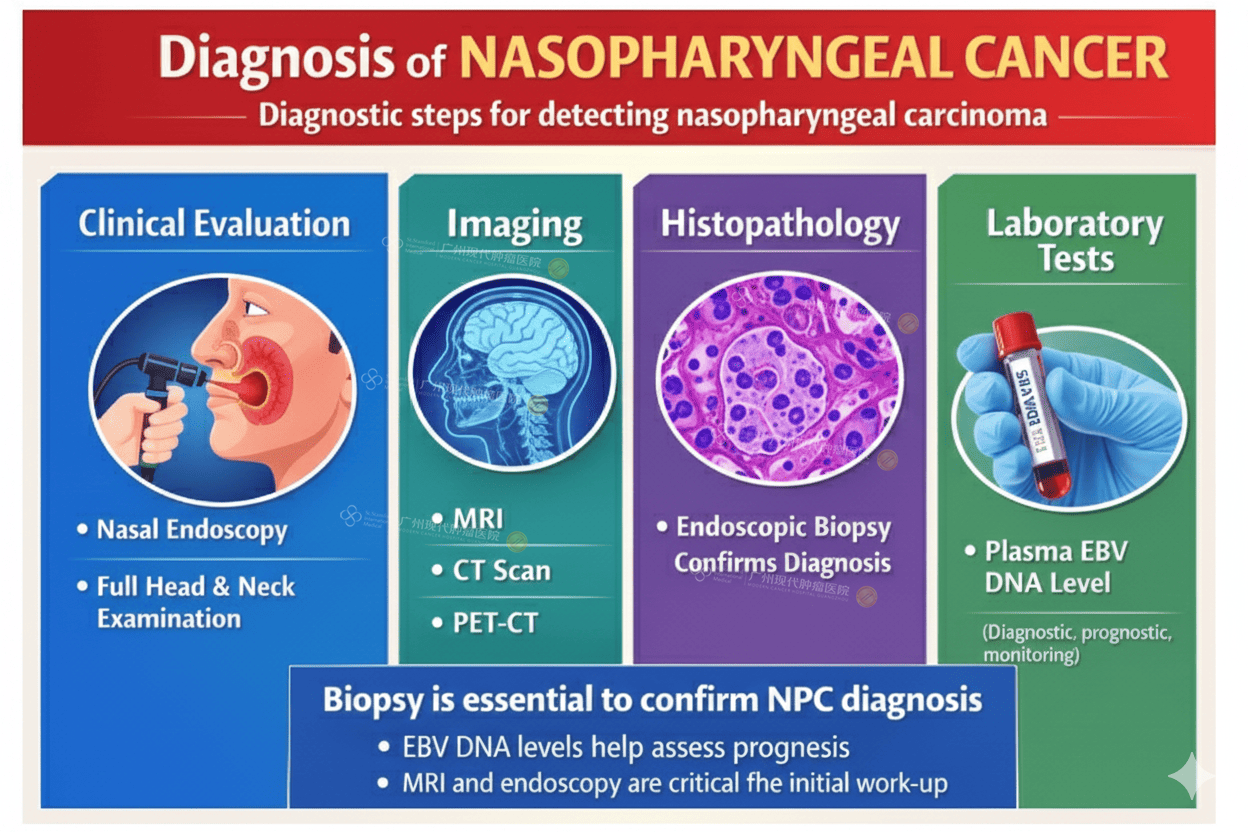
Diagnosis
Clinical Evaluation
Nasal endoscopy
Full head & neck examination
Imaging
MRI – best for local tumor extent and skull base invasion
CT scan – bone involvement
PET-CT – staging and distant metastasis
Histopathology
Endoscopic biopsy confirms diagnosis
Laboratory Tests
Plasma EBV DNA level (useful for diagnosis, prognosis, and monitoring treatment response)
Facts (FAQ)
Q1: Is nasopharyngeal cancer common in Malaysia?
Yes. Malaysia is considered an endemic region, especially among Chinese males.
Q2: Is NPC linked to smoking?
Smoking is a minor risk factor compared to EBV and diet.
Q3: Can NPC be cured?
Yes. NPC is one of the most curable head and neck cancers, even at advanced stages.
Q4: Can EBV blood test detect NPC early?
It can help with screening in high-risk populations but is not a standalone diagnostic test.
Q5: Does NPC recur?
Recurrence is possible, especially within the first 3 years. Long-term follow-up is essential.